Chapter 9 Biological Safety (Part 2)
F. Decontamination
1. GENERAL PROCEDURES FOR DECONTAMINATION OF WASTE
The most consistent and effective way to decontaminate biological waste is autoclaving. Autoclaving is fast and removes any ambiguity as to whether the decontamination process has been completed. For these reasons, and to eliminate concerns for health and safety among our staff and the community, we recommend that all biological materials except materials containing radioactive materials, carcinogens or hazardous volatile chemicals be disinfected by autoclaving prior to disposal, even though Biosafety Level 1 materials do not strictly require this method of disinfection.
All laboratories generating potentially biohazardous waste need to maintain appropriate containers to dispose, carry, and autoclave this waste. These items are available from CLS. It is expected that most of the waste generated will be disposable. For glassware and reusable items, it will be the responsibility of each laboratory to maintain separate autoclavable containers in which these materials can be autoclaved. After being autoclaved, these reusables should be rinsed before they are sent through the normal washing cycle.
For decontamination of table tops and surfaces, it is recommended that liquid decontaminating agents such as amphyl, broccal or other liquid disinfectants listed in Section F3 be used. As with the autoclave bags and containers, these items are available through the CLS stock room.
Waste which contains radioactive and/or carcinogenic or other hazardous compounds in conjunction with any biological samples should, if possible, be disinfected by chemical means (see Section F3), then discarded in appropriately labeled radioactive/chemical waste containers, i.e. biohazardous materials listed in addition to hazardous chemical and/or radioisotopes. This waste will be handled appropriately by HSEO. NEVER decontaminate biohazardous waste containing carcinogens, hazardous volatile chemicals, or radioisotopes by autoclaving. Contamination of both personnel and equipment may result. For further information on biohazardous samples that also contain carcinogens, hazardous chemicals or radioisotopes, see Sections E5 and E6, respectively.
2. HANDLING SPILLS
In any laboratory operation, the possibility of a spill exists. A thorough understanding of the potential hazards of the experiment as well as careful planning of a spill response protocol will help minimize personal injury and property damage.
While the severity of the accident will dictate the response required, the following general approach is recommended.
2.1 FIRST PRIORITY: PROTECT PERSONNEL
-
Notify your supervisor and the Security Control Centre (8999) from the nearest phone. Do not contaminate the phone.
-
Notify all personnel in the immediate area. Evacuate the immediate room or area if the accident is hazardous to others or if you are in doubt about the extent of the hazard.
- If the agent involved may be hazardous when inhaled, hold your breath as much as possible. Remove contaminated clothing and shoes and leave the area. Wash hands, face and other contaminated portions of the body with appropriate disinfectant and soap. If eyes have been contaminated, flush with water for 15 minutes.
- Secure the area of the spill and prevent people from entering the area. Place a sign at the entrance specifying the type of accident, the agent(s) involved, date and time of the accident, name of person to contact prior to entering the area.
2.2 SECOND PRIORITY: PROTECT EQUIPMENT AND FACILITY THROUGH PROPER CLEANUP AND DECONTAMINATION
-
Proceed only after consultation with, and approval from HSEO.
-
Re-enter the area after allowing at least 30 minutes for aerosols to settle.
- If the spill takes place in the open laboratory, decontamination may range from flooding the area with an appropriate disinfectant to fumigating the entire room with disinfectant chemical vapor, depending on the nature and scale of the spill. Use of appropriate personal protective equipment varies according to the level of hazard involved. In general, it may involve some or all of the following: coveralls, gloves, shoe covers, head cover, and respiratory protection.
- If the spill takes place within a biological safety cabinet, initiate chemical disinfection procedures while operating the cabinet ventilation system to prevent the escape of the contaminants from the cabinet. Appropriate gloves should be worn. Use sufficient disinfectant to assure the disinfection of the drain pans and catch basins below the work surface. Lift the front exhaust grill and tray and wipe all surfaces. Wipe the catch basin and drain the disinfectant into a container. Items used during the cleanup should be autoclaved prior to disposal or normal cleaning. This procedure will not disinfect the filters, blower, air ducts or other interior parts of the cabinet. Contact HSEO for decontamination of the entire cabinet.
- If the spill involves a radioactive biohazardous material, the cleanup procedure may have to be modified depending on the relative risk assessment of the biological and radiological hazards involved. Contact HSEO for specific details.
- If the spill involves a carcinogenic biohazardous material, special equipment and/or reagents may be required. Contact HSEO for specific details.
3. CHEMICAL DISINFECTANTS
Inactivation of microorganisms by chemical disinfectants may involve one or more of the following mechanisms: coagulation and denaturation of protein, lysis, and inactivation or destruction of an essential enzyme. Chemical disinfectants can be found in either gaseous or liquid form. Vapor and gaseous disinfectants are primarily useful in closed systems for sterilization purposes. The effectiveness of liquid chemical disinfectants hinges upon factors such as concentration, pH, temperature, contact time, penetration and dispersion. For these reasons, even when used under highly favorable conditions, complete reliance should not be placed on liquid disinfectants when sterility is required. Significant properties of common chemical disinfectants are summarized below. Be alert to the flammable nature of some disinfectants, and use accordingly.
3.1 ALCOHOL
Ethyl or isopropyl alcohol in a concentration of 70-80% by weight is often used as a disinfectant. Alcohols denature proteins and are somewhat slow in their germicidal action. They are good general-use disinfectants, but they exhibit no activity against bacterial spores.
3.2 CHLORINE
This halogen is a universal decontaminant active against all microorganisms, including bacterial spores. Chlorine combines with protein and rapidly decreases in concentration in its presence. Free, available chlorine is an active element. It is a strong oxidizing agent, corrosive to metals. Chlorine solutions will gradually lose strength, so fresh solutions must be prepared frequently. Sodium hypochlorite is usually used as a base for chlorine decontaminants. An excellent decontaminant can be prepared from household or laundry bleach. These bleaches usually contain 5.25% available chlorine or 52,500 ppm. Diluted 1 to 100, the resulting solution contains 525 ppm of available chlorine, and if a non-ionic detergent such as Naccanol is added in a concentration of about 0.7%, a very good decontaminant is created.
3.3 IODINE
The disinfectant characteristics of chlorine and iodine are similar. One of the most popular groups of disinfectants used in the laboratory is the iodophors, and of this Wescodyne is perhaps the most widely used. The dilution of Wescodyne recommended by the manufacturer ranges from 1 oz in 5 gal of water yielding 25 ppm of available iodine to 3 oz in 5 gal yielding 75 ppm. At 75 ppm, the concentration of free iodine is 0.0075%. This small amount can be rapidly taken up by extraneous protein. Clean surfaces or clear water can be effectively treated by 75 ppm available iodine, but difficulties may be experienced if any appreciable amount of protein is present. For washing hands or for use as a sporicide, it is recommended that Wescodyne be diluted 1 to 10, or 10% in 50% ethyl alcohol. This will yield 1,600 ppm of available iodine; a relatively rapid inactivation of all microorganisms will occur.
3.4 QUATERNARY AMMONIUM COMPOUNDS OR QUATS
After years of testing and use, there is still considerable controversy about the efficiency of the “Quats” as disinfectants. These cationic detergents are strongly surface-active, and this detergent property makes them good surface cleaners. They will attach to protein; so, dilute solutions of Quats will lose effectiveness in the presence of proteins. The Quats tend to clump microorganisms and are neutralized by anionic detergents, such as soap. They are bacteriostatic, tuberculostatic, sporostatic, fungistatic, and algistatic at low concentrations. They are bactericidal, fungicidal, algicidal, and virucidal against lipophilic viruses at medium concentrations, but they are not tuberculocidal, sporocidal, or virucidal against hydrophilic viruses even at high concentrations. The Quats have the advantages of being odorless, nonstaining, noncorrosive to metals, stable, inexpensive and relatively non-toxic. Caution should be used when handling concentrated Quats; even a small droplet splashed into the eyes may cause blindness. Be sure to wear safety glasses and proper personal protective equipment when handling these disinfectants.
3.5 FORMALDEHYDE
Formaldehyde for use as a disinfectant is usually marketed at about 37% concentration of the gas in water solution, referred to as formalin, or as a solid polymerized compound, paraformaldehyde. Formaldehyde in a concentration of 5% active ingredient is an effective liquid disinfectant. Formaldehyde loses considerable disinfectant activity at refrigeration temperature, 4oC. It is pungent and irritating in odor and is a confirmed human carcinogen. Formaldehyde vapor generated from formaldehyde solution is an effective space disinfectant for sterilizing rooms or buildings. Formaldehyde gas can be generated by heating paraformaldehyde to de-polymerise it. In the absence of high moisture content in air, the gaseous formaldehyde released forms less polymerized residues on surfaces and requires less time to clear treated areas of fumes than formaldehyde released in the vapor state. Formaldehyde vapors and gas can elicit hypersensitivity and irritation. They are also toxic and lachrymatory. Dilutions should be made in a chemical fume hood. Respiratory protection may be necessary. Formaldehyde vapours are flammable and proper precautions should be exercised to prevent explosion when working with this material.
3.6 PHENOL
Phenol itself is not often used as a disinfectant. The odor is somewhat unpleasant, and a gummy residue remains on treated surfaces. This is especially true during steam sterilization. Although phenol itself may not be in widespread use, phenol homologs and phenolic compounds are bases of a number of popular disinfectants, such as Lysol. The phenolic compounds are effective disinfectants against some viruses, rickettsiae, fungi and vegetative bacteria. The phenolics are not effective in ordinary use against bacterial spores. Concentrated phenolics should be used carefully; even a small droplet splashed into the eyes may cause blindness. Phenolics are readily absorbed by the skin; splashes can lead to both local irritation, severe burns, and systemic poisoning. Consequently, safety glasses and other proper personal protective equipment should be worn.
3.7 OTHER VAPORS AND GASES
Besides formaldehyde, other decontaminant vapors and gases include ethylene oxide, peroxyacetic acid, hydrogen peroxide, beta-propiolactone, methyl bromide, and ethylene amine. When they are used in closed systems and under controlled conditions of temperature and humidity, excellent decontamination can be obtained. Ethylene oxide is convenient to use, versatile and noncorrosive, however, it is highly toxic and has been identified as a suspected carcinogen and its residuals must be removed by aeration. Peroxyacetic acid is corrosive for metal and rubber. Beta-propiolactone in the vapor form acts rapidly against bacteria, rickettsia and viruses. It has a half-life of 3-5 hours when mixed with water, is easily neutralized with water and lends itself to removal by aeration. However, beta-propiolactone is also a suspected carcinogen. Vaporized hydrogen peroxide (VPH) has been used in pharmaceutical industries for disinfection, and has the advantage of not leaving any undesirable residue behind, because it decomposes to oxygen and water. It has also been used for disinfection of biological safety cabinets. VPH has a potential of being applied to other disinfection applications.
3.8 CAUTIONS REQUIRED WHEN APPLYING CHEMICAL DISINFECTANTS
When handling concentrated stock solutions of certain disinfectants, be aware of the potential hazards and exercise due caution. Concentrated quaternary and phenolic disinfectants are particularly harmful to the eyes. Even a small droplet splashed in the eyes may cause blindness. Absorption of phenolic compounds by the skin can lead to local irritation, severe burns, and to systemic poisoning. Chronic or prolonged exposure to phenol may cause headache, dizziness, difficulty in swallowing, diarrhea, vomiting, shock, convulsions, and death. Safety glasses and proper personal protective clothing should be worn to avoid corrosion and depigmentation of the skin. Good ventilation is required when working with phenol to minimize inhalation.
Vapor of formaldehyde can elicit hypersensitivity and irritation. It is also toxic. When making dilutions, work in a chemical fume hood. Respiratory protection may be necessary. Formaldehyde vapor is flammable and explosions can result so proper precaution should be exercised. In addition to considering the target organism, when choosing a chemical disinfectant also consider the potential chemical reactions between the disinfectant and the chemical components of the material to be disinfected. For example, the use of a chlorine-based disinfectant in a system containing radioactive iodine will result in the release of gaseous radioactive iodine. As a second example, mixing formaldehyde with a system containing hydrochloric acid will result in the generation of bis(chloro-methyl)ether, a potent human carcinogen.
Any question on the selection of an appropriate disinfectant should be directed to HSEO.
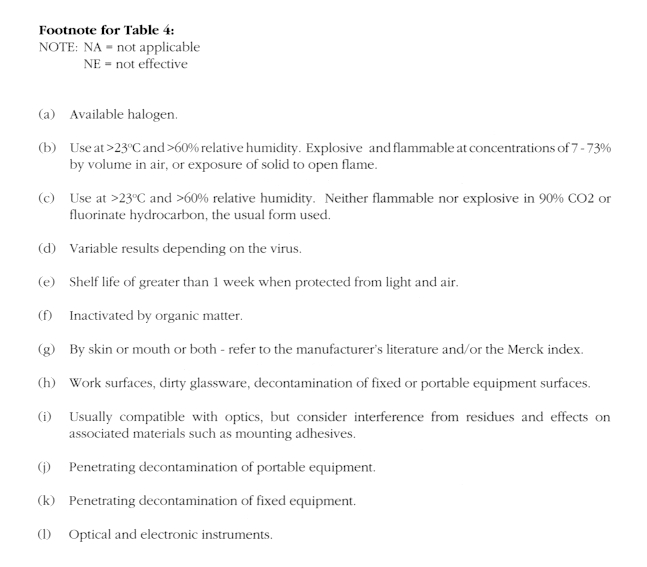
Pertinent characteristics and potential applications for several categories of chemical disinfectants most likely to be used in the biological laboratory are summarized in Table 4. The suggested practical concentrations and contact times may differ markedly from the manufacturer’s recommendations. A high degree of protection of microorganisms by organic matrices has been assumed, and a sterile state has not been assumed to result from application of the indicated concentrations and contact times. It should be emphasized that these data only indicate efficacy under artificial test conditions. The efficacy of any of the disinfectants should be conclusively determined by individual investigators. It is readily evident from Table 4 that each of the disinfectants has a range of advantages and disadvantages as well as a range of potential for inactivation of a diverse microflora. Equally evident is the need for compromise as an alternative to maintaining a large collection of different disinfectants.
TABLE 4 SUMMARY OF PRACTICAL APPLICATIONS OF CHEMICAL DISINFECTANTS

4. PHYSICAL AGENTS OF DISINFECTION
4.1.A. HEAT
The application of heat, either moist or dry, is recommended as the most effective method of sterilization. Steam at 121oC under pressure in the autoclave is the most convenient method of rapidly achieving sterility. Dry heat at 160o to 170oC for periods of 2 to 4 hours is suitable for destruction of viable agents on impermeable nonorganic materials such as glass, but is not reliable in even thin layers of organic or inorganic material that can act as insulation. Incineration kills microorganisms and serves as an efficient means for disposal. Sample requirements for steam autoclaving of some materials are listed below:
-Laundry: 121oC for 30 minutes with 15 minutes pre-vacuum of 27 inches of Hg.
-Trash: 121oC for 1 hour with 15 minutes pre-vacuum of 27 inches of Hg.
-Glassware: 121oC for 1 hour with 15 minutes pre-vacuum of 27 inches Hg.
-Liquids: 121oC for 1 hour for each gallon.
4.1 B. AUTOCLAVE USE
Safe and effective use of autoclaves for disinfection requires:
-
Use of proper bags and containers, with adequate openings for steam penetration and pressure release.
- Water should be added to bags containing dry materials such as paper goods.
- Caps on flasks and tubes should be left off or loosely fastened.
- Biohazard level 2 materials should be double bagged.
- Label materials with experimenter’s name, lab room number, autoclave status, and, if appropriate, presence of biohazard level 2 materials.
- Exclude radioactive or carcinogenic materials, or materials containing more than trace amounts of solvents or corrosive materials, such as phenol, chloroform, trichloroacetic acid, chlorox.
- Load the autoclave properly. Do not overload or pack too tightly.
- Carefully remove materials at the end of the autoclave cycle. All pressure should have been released. On opening the autoclave, hands, arms, and face should be protected from released steam; gloves, lab coat, and protective eye wear should be worn.
- Always check temperature and pressure readings and/or records of autoclave to ensure the target levels are reached. Keep records of autoclave runs as proof of proper waste disinfection.Conduct periodic performance test using thermophilic bacterial spores test kits available from CLS. Keep records as proof of proper waste management practice.
4.2 NON-IONIZING RADIATION
Ultraviolet radiation (UV) is a practical tool for inactivating viruses, mycoplasmas, bacteria, and fungi. UV is especially useful for the destruction of airborne microorganisms on exposed surfaces or for the treatment of products of unstable composition that cannot be treated by conventional methods. Its usefulness as a sanitizer is limited by its low penetrating power. UV is primarily used in air-locks, animal holding areas, ventilated cabinets, and laboratory rooms during periods of non-occupancy to reduce the levels of viable airborne microorganisms and to maintain good air hygiene. An intensity of 40 microWatt /cm 2 at 253.7 nm is generally used for germicidal purposes. The eyes and skin can be damaged by exposure to direct or strongly reflected ultraviolet radiation. Adequate eye and skin protection must be worn when working in an area being irradiated. A UV-blocking face shield is the best protection for eyes and face. If a face shield is not available, safety glasses with side shields or goggles with solid side pieces may be worn for eye protection. Skin protection is afforded by face shields, caps, gloves, gowns, and other appropriate equipment.
4.3 IONIZING RADIATION
The germicidal action of x-radiation has been known for years. Gamma radiation at very high doses is used for the destruction of microorganisms in some food products. However, ionizing radiation generally is not a practical tool for laboratory use.
G. Common Research Procedures That Inactivate Biohazards
Certain experimental procedures inactivate biohazardous agents. As a consequence, subsequent work can be derated with respect to Biosafety Level. Examples of commonly used, inactivating procedures are:
- Fixation of tissues or cells as in cytogenetic studies or other fixed-cell analyses: Included here are the standard fixatives, such as 70% ethanol and mixtures of glacial acetic acid and methanol, as well as procedures that lead to extreme cross-linking of proteins, such as treatments with dimethylsuberimidate.
- Disruption of normal agent integrity, as in the extraction of DNA, RNA or protein.
- Exposure to extreme, nonphysiological conditions, e.g. pH, salt, radiation, and dessication.
NOTE: These procedures vary in their efficacy of inactivating biohazards. Derating of subsequent work should be done with caution.
H. Containment Equipment And Supplies
1. Biological Safety Cabinets
The properties and the classification of the different types of biological safety cabinets are discussed in detail in the CDC-NIH document Primary Containment for Biohazards: Selection, Installation and Use of Biological Safety Cabinets (http://www.cdc.gov/od/ohs/biosfty/bsc/bsc.htm).
The performance of biological safety cabinets will be verified at the time of installation, and thereafter on a yearly basis or whenever they are moved. This service is provided by CMO Laboratory Services. You may also contact HSEO for any question about the performance or certification of biological safety cabinets.
As with any piece of laboratory equipment, personnel must be trained in the proper use of the biological safety cabinet. Activities that disrupt the inward flow of air through the front access of the cabinet should be minimized. Repeated movement of worker's arms in and out of the work chamber, opening and closing of doors to the laboratory, improper placement or operation of materials or equipment in the work chamber, or brisk walking past the biological safety cabinet facilitate escape of aerosolized particles from within the cabinet. Use of flames should be limited. Electrical loop incinerators are recommended for bacteriological loop sterilization.
2. Containment Protection For Vacuum Systems
The aspiration of tissue culture media from monolayer cultures or of supernatants from centrifuge samples into primary collection flasks is a common laboratory procedure. Protection should be provided against drawing aerosols of hazardous chemical or biological materials or overflow fluid into the vacuum system. This protection is provided by the use of an air filter in the line immediately leading into the house vacuum line and an overflow flask for liquids between the collection flask and the air filter.
To assemble this protective apparatus, use flexible tubing of appropriate inside diameter for the flask and filter fittings and of sufficient wall thickness for the applied vacuum. Filter flasks of capacities from 250 to 4000 ml may be used for the overflow flask, depending on the available space and the amount of fluid that could be accidentally aspirated out of the collection flask. The overflow flasks should contain a disinfectant solution appropriate for the biohazardous material under study. It is essential that an antifoam agent, such as Dow Corning Antifoam A, be added to the overflow flask, since bubbling of air through the disinfectant probably will cause considerable foam which, if allowed to reach the filter, will shut off the vacuum.
If the filter becomes contaminated or requires changing, the filter and flask can be safely removed by clamping the line between filter and vacuum source. The filter and flask should be autoclaved before the filter is discarded. A new filter can be installed and the assembly replaced.
This protective apparatus for the vacuum system is shown in Fig. 1. A cartridge-type HEPA filter provides an effective barrier to passage of aerosols into the house vacuum system. The filter has a capacity to remove airborne particles 0.3 micron in size at 99.97% efficiency.
Figure 1. Protective Apparatus for the Vacuum System
I. Medical Surveillance For Biohazard Workers
Biohazard workers are defined as those staff members, contract workers, long-term visitors and students who engage in the following activities: working with any Risk Group 2 biological agents or cells (Risk Group 3 and 4 agents are NOT ALLOWED at HKUST), processing samples of tissues or body fluids (blood, serum, or semen) from humans or other primates, or handling of laboratory animals for care or experimentation. The principal investigator is responsible for informing HSEO in advance when any employee will be working with biohazardous materials. This will include work with microorganisms: isolation, culturing, mutation testing; work with virus-infected cells or isolated viruses; all forms of genetic engineering, and work involving handling of animals by animal care staff and research staff. A roster of biohazard workers will be maintained by HSEO. HSEO management must update this listing annually, and when new personnel begin work with biohazards.
Minimum medical surveillance for biohazard workers includes a review of medical records, a periodic examination of the employee’s health, with appropriate review of activities being performed and any suspected significant exposure. Medical records should include reports of any instances of accidental ingestion, inhalation, or skin penetration of biohazardous material. Employees working with potential biohazards must report any exposures immediately to HSEO. Employees being treated with immunosuppressive drugs shall be excluded from biohazard work for the duration of treatment, and the treating physician must provide a statement that the employee’s immune status is normal prior to return to biohazardous work. Modification of work regimens during pregnancy shall be determined on a case-by-case basis.
Staff who work with potentially pathogenic microorganisms, with human cells or other samples that may contain infectious agents, and those who care for or work with experimental animals, are requested to have a serum sample banked by HSEO as a baseline for future assay in the event of accidental exposure. Additional samples will be obtained for assay in the event of a suspected exposure. Blood samples will be drawn and serum prepared for storage in a labeled container in a 20oC freezer. Contact HSEO for further information.
Staff who work with human samples of any kind will be offered a course of vaccine (3 injections over 6 months) against hepatitis B virus to prevent illness in the event of accidental infection.